Creating a tool to record data across multiple clinical contexts from paramedics to high dependency ward rounds for a new disease and getting the ‘product’ live and integrated with cornerstone systems within the largest health board in Europe was a unique challenge. The multidisciplinary team needed to develop new ways of online collaboration to ensure successful delivery. The challenge was further compounded as the tool need not only to support structured clinical assessment across multiple clinical environments but also visualise data for operational management and support academic clinical researchers seeking to develop new insights into a novel disease process.
Collaborating across boundaries requires building shared understanding not only of the goals of the project but of the language of each group, especially when each disciplines have three-letter acronyms to describe every process. Unpacking clinical practice requires a forensic breaking down of each step in the process and creating a shared understanding of underlying reasoning for each decision. Creating a tool to record clinical interactions for a disease enabling health care professionals to record their critical decision making comes with a unique set of challenges. Worldwide our understanding of C-19 continues to evolve at pace with rapid iterations of the C-19 app prototypes not only based on feedback from clinicians across Scotland but also incorporating the current evidence base as it was published.
The team at Daysix and EmQuire have an established strategy to breakdown these requirements and create a shared understanding. Ben @daysix borders on persecutory when exploring the need for additional data fields and balancing the needs of granular data for researchers against user engagement on the shop floor. The development of the Trauma App (www.thetraumaapp.com) has enabled a process of rapid prototyping and iteration as the clinical and development team seek to create the optimal solution . The ability to shortcut the need to explain heart rate parameters, what inotropes are (drugs to improve blood pressure) or what a RSI is (putting a patient off to sleep) accelerates the design process enabling wireframes to be shared to gain clinical consensus.
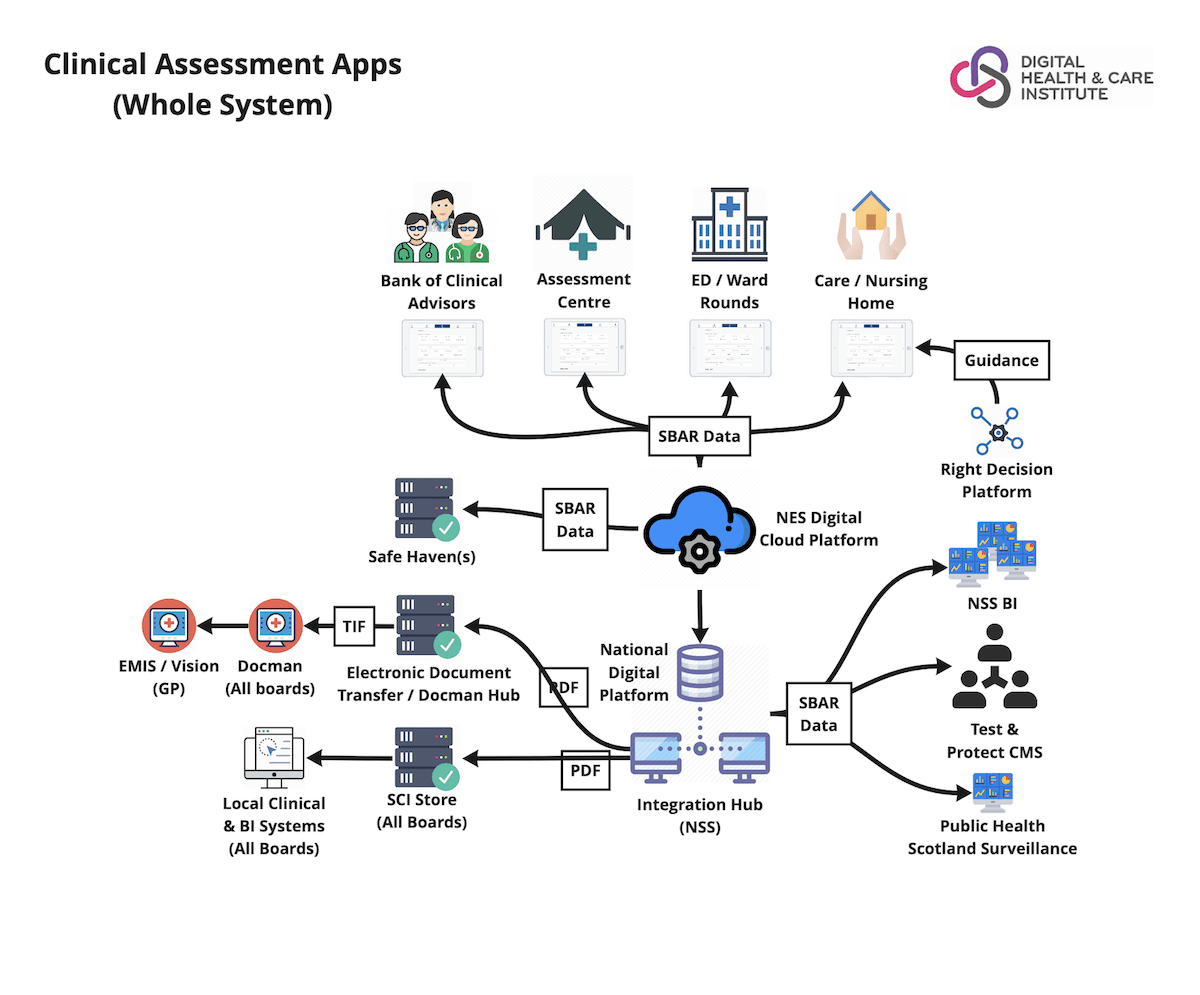
The DHI and NES were able to rapidly describe the wider clinical and data workflow using a variety of online tools. Don McIntyre and Jay Bradley led a number of workshops using MIRO to visualise these work flow to ensure that all collaborators across the team understood the requirements to ensure data and patients could flow through a new pathways.
The daysix clinical wireframe tool and Miro for Clinical pathways enabled teams to explore edge cases and identify key areas of responsibilities. Anna Armstrong from NES used JIRA to collect stories and create a backlog for the key developers Ian Wallace and Gavin Hickford to rapidly understand the clinical context and why it was important to document the time a patient was able to be proned.

